So many times when parents are sitting with me during an initial consultation to discuss their child’s inability to eat, they will ask the inevitable question, “What do you think caused this?”
As humans we all have this inherent need to understand the cause of problems.
This is logical, but how do you fix something if you don’t know what is causing it? Parents are seeking for the cause in the hopes of applying a “tried and true” course of treatment. In most cases, however, pediatric feeding difficulties are so complex that it seems virtually impossible to identify and address all of the many “moving parts”.
Now I am NOT going to get into the many different diagnostic categories and classifications that exist and that I have heard, read about and treated throughout my nearly 21 years of practice – organic, non-organic, behavioral, self-limiting – whatever it is – the common thread is that there are many children out there who cannot eat, and their parents are DESPERATELY in need of help. Plainly put, a feeding disorder is a multi-faceted problem. These separate “facets” interact with each other, thus creating “the perfect storm”. Each facet of the problem needs to be addressed directly but yet in sync with all other presenting facets, just like a group of dancers performing together in a well choreographed dance. A good feeding therapist is smart enough to know his or her limits – and just like a dancer attempting to practice a routine alone for weeks and then expect to perform collaboratively with 10 other dancers on opening night – treating a pediatric feeding patient without ever collaborating with the child’s caregivers, teachers, or other members of the professional/healthcare team is a recipe for disaster. The routine WILL fall apart!
Good feeding therapy will uncover all of the layers of the problem.
It will examine all facets, the underlying medical, psychological, structural, motor, and/or sensory dysfunction. It will analyze the undesired behavioral responses – and I stress the word RESPONSE, only because I have never met a child who has a feeding disorder that is caused only by behavior (contrary to the belief of many well-meaning professionals). Feeding therapy should not be limited to only 30 minutes in a clinical setting and then checking back at the same time and same place the following week. It is a time to ask many questions to a parent about home routines and provide a clear plan for the child (and parent) to follow at home, while discovering the unique needs of the child (a one size fits all NEVER works). All of this should be well coordinated with other members of the child’s team to design a multidisciplinary treatment plan. It is lastly about working with parents and making them understand that they bear just as much responsibility in the process as all of the professionals working with their child. The “please fix my child” attitude needs to shift to “let’s get this done as partners”!
Successful outcomes are possible!
When objectives are realistic, all members of the team (inclusive of the parent) understand their respective roles and all underlying aspects are uncovered, gains are achievable. It will take time depending upon the nature or complexity of the underlying issues, but outlining realistic time expectations will lead to less frustration and disappointment. Keep charts to document even the smallest of amount of success. This will help all participants in the process “see” the progress even when the progress is too slow to feel the effect on a daily basis. Above all never lose hope, for every child brings a new opportunity to learn, a new opportunity to help and a new opportunity to watch them soar above any obstacle. ❤️
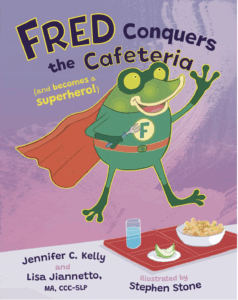
Lisa Jiannetto-Surrusco, MA, CCC-SLP is a practicing Speech-Language Pathologist in the NYC/NJ area. She is the owner of Reach for the Stars, LLC, in Cranford, NJ, and is also the Clinical Director Speech Therapy and Evaluation Services at The Perfect Playground in Staten Island, NY. She has over 21 years of experience treating children with feeding issues. Published July 13, 2019